Misunderstood Markers of Health – What’s in a Number?
Dr Sean Wheatley, MSc, PhD. Science and Research Lead, X-PERT Health.
Sean.Wheatley@xperthealth.org.uk
Know Your Numbers
Knowing your key health results can be very important. They help to provide an understanding of what is going on in your body. This is valuable information to help us make informed lifestyle choices, and/or to guide potential interventions where necessary.
They are only useful if we know what they mean though.
Key Limitations
It is common for people to be presented with their results without any context or discussion of what they mean. This is often because of the lack of time healthcare professionals have to spend with their patients, due to fundamental flaws with the current system. The end result is confusion, and a risk that the individual will not have enough information to help them make choices that are right for them.
What makes this worse still is that some of the most commonly used health markers have limitations. This means that even a general understanding of what they mean might not be nuanced enough to guide decision making.
Two examples of this are body mass index (BMI) and glycated haemoglobin (HbA1c). Although used for different things, these measurements have a key similarity: they both provide a generally useful overview of health, but do not provide all of the relevant information on their own.
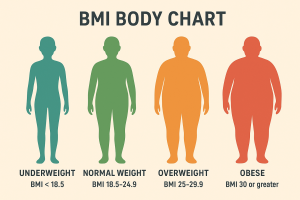
Example 1. BMI
As most people know, BMI is a marker of body size. Most people are also aware that there are some limitations with BMI, including that:
- It does not tell us anything about body composition, e.g., how much of our weight is fat and how much is muscle.
- It does not tell us anything about where fat is stored in the body, e.g., how much is in and around internal organs, how much is around our waist, and how much is stored elsewhere.
As a result of these limitations, some people disregard their BMI entirely. It is easy to ignore a health result you don’t like if there are reasons to believe it is flawed.
However, most people with a high BMI will be storing excess fat in their body. In most cases this will increase the risk of unwanted complications, such as type 2 diabetes and heart disease.
So, although we would ideally have other health results (e.g., a measurement of waist size) to use alongside BMI to help us understand whether an elevated score is likely to correspond to an increased risk of health problems, that does not mean we should completely ignore BMI on its own just because it doesn’t provide the full picture.
Example 2. Glycated Haemoglobin, or “HbA1c”
HbA1c provides a general indicator of blood glucose control. It is the health marker that is usually used to diagnose prediabetes or type 2 diabetes. It is also used to monitor the management of these conditions where they have already been diagnosed.
Similarly to BMI, HbA1c does provide a good general marker of health. But also like BMI, it has limitations. In this case, although it provides a ballpark “average” figure, it does not provide any information on patterns of blood glucose levels, e.g., whether they fluctuate significantly during the day, whether there are particular times where they are higher than others, or whether there are specific things that cause them to rise particularly high (e.g., certain foods or activities).
Again though, in most people with a raised HbA1c it is likely that something is going on that would ideally be addressed, through lifestyle changes or with medication (for example). So as with BMI, just because there are limitations that does not mean we should ignore it. But also as with BMI, we would ideally have access to other information (e.g., continuous glucose monitoring data) to help refine our understanding of what is happening.
So, what’s the bottom line?
Context is king, but sometimes we don’t have all the information we might want to make an informed decision. In these cases, understanding what your health results actually mean, including what they do not tell you is important. We should not however entirely dismiss any of our results because they have some limitations, or because we do not like them! Almost all health markers have some flaws, but they often still provide some potentially useful insight.
If you are still unsure what to make of any of your results, or believe they might be misleading, then ask your healthcare team! They are ultimately there to help you make decisions that are right for you, taking into account not only your health results but also your needs and preferences. In some cases that might mean you want or need to talk through your options a little further, and in others it might mean extra testing is needed to help fill in any gaps.
Postscript – A Quick Note on Risk Clustering
Although I stand by the points made above, about how even a flawed health marker can provide some useful information, it is often better to look at the clustering of risk factors rather than to obsess with individual markers anyway. A single health result outside of a “desirable” range might be difficult to interpret with confidence, in line with the points made above, but if there are multiple results outside of a “desirable” range then this is likely to be a reliable sign that some kind of action is needed.
For example, if your BMI was raised, but everything else was “normal”, then you might be unsure as to whether or not action is needed. But if your BMI, your HbA1c and your blood pressure were all raised, then this clustering of risk factors would suggest that some form of lifestyle change or medical intervention would be of benefit.
Download X-PERT Health Monitoring Health Form